Rheumatologist: When / why?
 Rheumatism (from greek verb “ρέω” that means flow, and suffix - ism) are called the pains and general discomfort of the musculoskeletal system. It often afflicts many people around us, and it has even been recognized as the leading cause of visits to the doctor and the second cause of drugs prescription. If one consider that is the main reason of acute and chronic disability, one can understand the impact of rheumatic diseases on the patient, but also the community.
Rheumatism (from greek verb “ρέω” that means flow, and suffix - ism) are called the pains and general discomfort of the musculoskeletal system. It often afflicts many people around us, and it has even been recognized as the leading cause of visits to the doctor and the second cause of drugs prescription. If one consider that is the main reason of acute and chronic disability, one can understand the impact of rheumatic diseases on the patient, but also the community.
The Rheumatology has as its object more than 200 diseases, which are mainly manifested by signs and symptoms of the human musculoskeletal system, but they can also take systemic nature by infecting more organs (lungs , kidneys , eyes , nervous system , etc. ). Thus, symptoms that will lead the patient to a specialist rheumatologist often can be:
-
Pain and swelling of joints
-
Limitation in the motion range of a joint
-
Pain and stiffness of the spine
-
Sensitive and weak muscles
but also less common such as:
-
Various rashes in conjunction with the musculoskeletal complaints (e.g. psoriasis)
-
Diffuse mucosal dryness (dry eyes, mouth, skin) and a multitude of other symptoms that one is initially unable to afford to rheumatism.
In any case, the rheumatologist is called to see each patient spherical and as a separate entity with the aim, reaching the diagnosis, to relieve him of complaints that hinder his daily life and sometimes make him physically and mentally helpless.
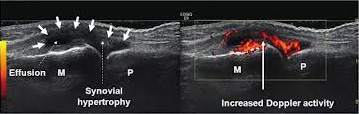
Fortunately, the last 10-15 years, rapid advancements have been made in Rheumatology, in both the diagnostic and the therapeutic part. It is no coincidence that together with the Oncology they are in the top of research drawing worldwide. For example, with the use of ultrasound, we are able to reliably and early check joints and periarticular tissues for inflammatory and / or degenerative conditions, whilst we are given the possibility to intervene therapeutically with ultrasound guided injections. Also, newer drugs developed based on the understanding of the pathogenesis of rheumatic diseases, enable early treatment before irreversible changes occur.
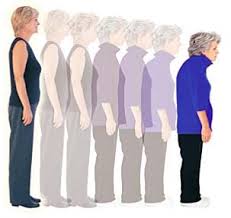
Distinguishing rheumatic diseases based on their pathogenicity, there are the autoimmune diseases, due to immune system disorders, and the degenerative diseases, that occur due to wear of physiological structures of joints, such as of cartilage in osteoarthritis. There are also the metabolic diseases of bones, such as osteoporosis with various causes. The autoimmune diseases are more rare, and usually have an earlier age of onset, such as 20 to 30 years for ankylosing spondylitis and systemic lupus erythematosus, and potentially more serious events.
Early intervention plays a key role in achieving remission or suspension of a disease progression and is an achievable target along with proper medication in combination with non-pharmaceutical measures, such as diet and exercise. Additional treatments, such as acupuncture, yoga and use of nutritional supplements, have a growing position in the disease treatment.
For more information about rheumatic diseases useful links are:
Greek Society for Rheumatology - www.ere.gr
Greek Company of Anti-Rheumatism struggle ( EL.E.AN.A. ) - www.arthritis.org.gr
Arthritis Foundation (USA)- www.arthritis.org
Arthritis Research Campaign (UK)- www.arc.org.uk